Medicines for idiopathic hypersomnia and narcolepsy
and avoiding interactions with hormone medicines, such as birth control, hormone replacement therapy, and gender-affirming therapy

and avoiding interactions with hormone medicines, such as birth control, hormone replacement therapy, and gender-affirming therapy
The table below shows medicines that are approved by the U.S. Federal Drug Administration (FDA) specifically to treat narcolepsy (*) or IH (†) and symptoms the medicines may improve. In the U.S., as long as a medicine is approved by the FDA to treat any condition, doctors may prescribe it “off-label” to treat other conditions.
Scroll right to see more columns
| Generic medicine names (example brand names) | Daytime sleepiness | Cataplexy | Sleep inertia | Sleep disruption |
|---|
| Generic medicine names (example brand names) |
|---|
| Modafinils* (such as Nuvigil) |
| Oxybates*† (such as Xyrem) |
| Pitolisant* (such as Wakix) |
| Solriamfetol* (such as Sunosi) |
| Amphetamines* (such as Adderall) |
| Methylphenidates* (such as Jornay PM) |
| Generic medicine names (example brand names) |
|---|
| Generic medicine names (example brand names) | Daytime sleepiness | Cataplexy | Sleep inertia | Sleep disruption |
|---|---|---|---|---|
| Modafinils* (such as Nuvigil) | ||||
| Oxybates*† (such as Xyrem) | ||||
| Pitolisant* (such as Wakix) | ||||
| Solriamfetol* (such as Sunosi) | ||||
| Amphetamines* (such as Adderall) | ||||
| Methylphenidates* (such as Jornay PM) |
The table below shows other medicines that may be used to treat IH or narcolepsy, and the symptoms they may improve, based on currently available evidence. None of these are FDA-approved specifically to treat IH or narcolepsy.
Scroll right to see more columns
| Generic medicine names (example brand names) | Daytime sleepiness | Cataplexy | Sleep inertia | Sleep disruption |
|---|
| Generic medicine names (example brand names) |
|---|
| Clarithromycin (such as Biaxin) |
| Flumazenil |
| Antidepressants (such as Prozac) |
| Bupropion (such as Wellbutrin) |
| Bupropion long-acting (such as Wellbutrin XL) |
| Protriptyline (such as Vivactil) |
| Selegiline (such as Emsam) |
| Atomoxetine (such as Strattera) |
| Reboxetine (such as Davedex) |
| Levothyroxine (such as Synthroid) |
| Baclofen (such as Lioresal) |
| Caffeine (such as No Doz, drinks) |
| Carnitine supplements (such as Carnitor) |
| Melatonin long-acting |
| Generic medicine names (example brand names) |
|---|
| Generic medicine names (example brand names) | Daytime sleepiness | Cataplexy | Sleep inertia | Sleep disruption |
|---|---|---|---|---|
| Clarithromycin (such as Biaxin) | ||||
| Flumazenil | ||||
| Antidepressants (such as Prozac) | ||||
| Bupropion (such as Wellbutrin) | ||||
| Bupropion long-acting (such as Wellbutrin XL) | ||||
| Protriptyline (such as Vivactil) | ||||
| Selegiline (such as Emsam) | ||||
| Atomoxetine (such as Strattera) | ||||
| Reboxetine (such as Davedex) | ||||
| Levothyroxine (such as Synthroid) | ||||
| Baclofen (such as Lioresal) | ||||
| Caffeine (such as No Doz, drinks) | ||||
| Carnitine supplements (such as Carnitor) | ||||
| Melatonin long-acting |
For more in-depth information about these medicines, such as side effects, mechanisms of action, and evidence for use, visit our healthcare professional web page, “Treating people who have idiopathic hypersomnia or narcolepsy.”
Currently, there are no medicines that specifically treat brain fog or automatic behaviors. However, treating daytime sleepiness may also help these symptoms.
Some PWH report fewer problems with sleep paralysis and hallucinations if they avoid falling asleep flat on their backs.
For sleep paralysis, specific forms of meditation may help.
Visit Project Sleep’s “Sleep Paralysis and Hallucinations” web page to get some other ideas and understanding that can help with these symptom
Amphetamines and their derivatives: Adderall, Adzenys ER, Adzenys XR, Biphetamine, Dexedrine, Dyanavel XR, Evekeo, Mydayis, ProCentra, Vyvanse, and Zenzedi
Reboxetine: Davedex, Edronax, Irenor, Norebox, Prolift, Solvex, Yeluoshu, and Zuolexin
Bupropion: Aplenzin, Budeprion SR, Budeprion XL, Buproban, Forfivo, Forfivo XL, Wellbutrin, Wellbutrin SR, Wellbutrin XL, and Zyban
Caffeine: No Doz
Carnitine: Carnitor
Clarithromycin: Biaxin, Biaxin XL
Flumazenil: Romazicon
Mazindol: Quilience
Methylphenidate formulations: Adhansia XR, Aptensio XR, Concerta, Cotempla XR-ODT, Daytrana, Focalin, Jornay PM, Metadate CD, Metadate ER, Methylin, Methylin ER, QuilliChew ER, Quillivant XR, Ritalin, Ritalin LA, and Ritalin SR
Armodafinil: Acronite, Armod, Armoda, Artivil, Modavital, Neoresotyl, Nuvigil, R-Modawake, and Waklert
Pitolisant: Wakix
Protriptyline: Vivactil
Selegiline: Eldepryl, Emsam, and Zelapar
Sodium oxybate: Alcover, Gamma-OH, Natrii oxybutyras Kalceks, Somsanit, and Xyrem
Lower-sodium oxybate: Xywav
Extended-release sodium oxybate: Lumryz
Solriamfetol: Sunosi
Duloxetine: Cymbalta, Drizalma Sprinkle, and Irenka
Levomilnacipran: Fetzima
Desvenlafaxine: Pristiq and Khedezla
Escitalopram: Lexapro
Fluoxetine: Prozac and Sarafem
Paroxetine: Brisdelle, Paxil, and Pexeva
Sertraline: Zoloft
Clomipramine: Anafranil
Protriptyline: Vivactil
 You may need to try different hypersomnia medicines and doses to find the treatment that works best for you
You may need to try different hypersomnia medicines and doses to find the treatment that works best for youAs you work with your doctor to try different hypersomnia medicines, here are some things to think about.
Some medicines may not work well for you.
You may need to use more than one medicine at a time (a combination of medicines).
Taking breaks every once in a while from wake-promoting medicines may help them to work better again. For example, some people find that taking a break on weekends is helpful.
Asking your doctor when you should feel better on your new medicine can help you figure out when or if you need to change your dose or treatment plan.
Some medicines work best when you take them at a specific time of day. Ask your doctor how many hours each medicine usually takes to start working and how long they’ll last during the day. This can help you plan when to take them.
Some medicines may have side effects, such as nausea, headaches, or raised blood pressure. Talk with your doctor about which side effects are the most common and which are the most dangerous. Ask about any side effects that worry you.
You may have no side effects at all, but there’s usually no way to find out without trying the medicine yourself.
![]() If you could become pregnant, talk with your doctor about the safety of your medicine during pregnancy and nursing. Visit our web page “Pregnancy and safe baby care.”
If you could become pregnant, talk with your doctor about the safety of your medicine during pregnancy and nursing. Visit our web page “Pregnancy and safe baby care.”
Learn more about side effects:
Many of the more common or important side effects are listed on our Treatment web page for doctors, which includes more in-depth information about hypersomnia medicines
For more information on side effects, visit Medline Plus.
Talk with your doctor about starting with a low dose and slowly raising it. This may help you to get a feel for:
What dose helps your symptoms
What dose gives you unwanted side effects
What dose gives the best balance between side effects and helping your symptoms
You may need different doses for different days, such as:
A usual dose for most days
A higher dose for days with worse symptoms or many activities planned
A lower dose for days when you don’t have much planned
If you menstruate (have a period):
You may need a higher dose for the 2 weeks before your period, when symptoms can be worse.
Some people with hypersomnias have shared that they have worse symptoms around their period, but there is no research evidence yet. Let your doctor know if this is true for you.
If you’re taking a combination of medicines and need to make changes, it’s usually best to change just one medicine at a time. Talk with your doctor before making any changes.
You still may not feel fully alert, even if you’re taking the medicines that work best for you. A good goal is to try to be most alert at important times of the day, such as during work, school, or while driving.
The Idiopathic Hypersomnia Severity Scale (IHSS) and Narcolepsy Severity Scale (NSS) are tools that you and your doctors can use to help measure how well a treatment is working to ease your symptoms. Depending on your diagnosis, you can take one of these questionnaires before and after you start a new treatment to see if your scores improve. The FOSQ (Functional Outcomes of Sleep Questionnaire) and ESS (Epworth Sleepiness Scale) are other options for people with any hypersomnia sleep disorder.
Getting support from other people with hypersomnias can help. You can join support groups (visit the Support group section on our “Quality of life tips” web page) or ask your doctor if they can give your contact information to other people who have taken the same medicines as you.
These hypersomnia medicines can affect how well medicines with hormones (estrogens, progestins, or testosterones) work:
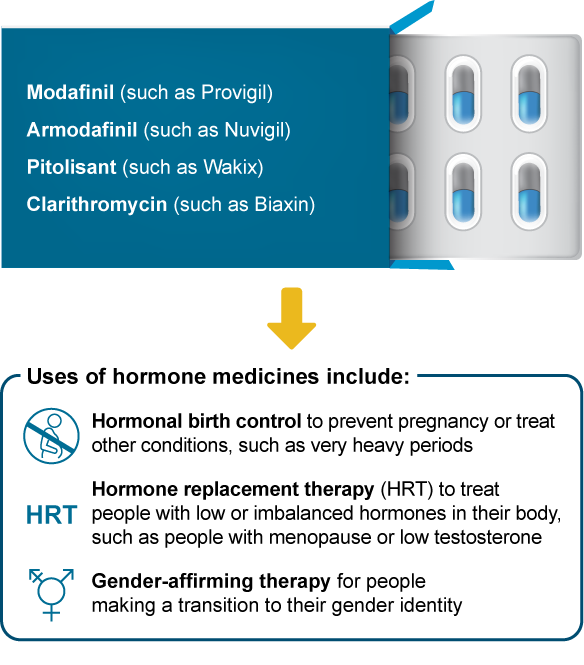
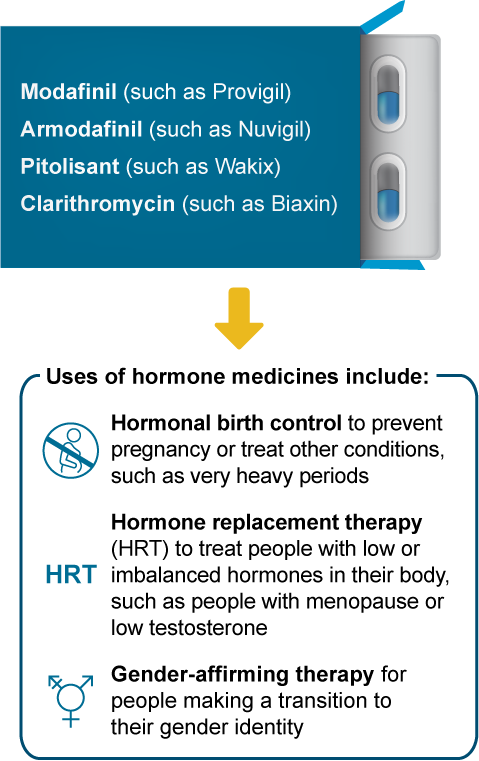
What may happen if I take these medicines together?
Less symptom control, such as not controlling hot flashes during menopause
A higher risk of pregnancy
Less medicine effectiveness, such as with gender-affirming therapy
More side effects, such as headaches or breakthrough menstrual bleeding
It’s usually safe to use these hypersomnia medicines with hormone medicines. To help ensure the hormone medicine still works well, you and your doctor may decide to:
Change your hypersomnia medicine to one that doesn’t interact with hormone medicines
Change the dose of your hormone medicine
Switch to a different method of birth control that isn’t affected, such as an IUD
Change your hormone dosing amount or schedule
Add a barrier method, such as also using a contraceptive diaphragm or condom

Scroll right to see more columns
|
Hormonal birth control options that can interact with hypersomnia medicines include: |
|
Hormonal birth control options that can interact with hypersomnia medicines include: |
| Birth control implant |
| Birth control pills |
| Birth control patch |
| Birth control ring |
| Emergency birth control |
|
Hormonal birth control options that can interact with hypersomnia medicines include: |
|
Hormonal birth control options that can interact with hypersomnia medicines include: |
| Birth control implant |
| Birth control pills |
| Birth control patch |
| Birth control ring |
| Emergency birth control |
Scroll right to see more columns
|
Other birth control options that don’t interact with hypersomnia medicines include: |
|
Other birth control options that don’t interact with hypersomnia medicines include: |
| Sterilization (vasectomy or tubal ligation) |
| IUDs |
| Progestin shots (such as Depo-Provera) |
| Condoms |
| Contraceptive diaphragms |
|
Other birth control options that don’t interact with hypersomnia medicines include: |
|
Other birth control options that don’t interact with hypersomnia medicines include: |
| Sterilization (vasectomy or tubal ligation) |
| IUDs |
| Progestin shots (such as Depo-Provera) |
| Condoms |
| Contraceptive diaphragms |
For more in-depth information on managing interactions between hypersomnia and hormone medicines, see the section “Some hypersomnia medicines interact with hormone medicines,” on our Treatment web page for doctors.
 Volunteering for clinical trials may allow you to try medicines that aren’t yet available in your home country nor approved for your diagnosis. Some clinical trials allow participants to continue taking the medicine for a period of time after the trial has ended. Clinical trials also help scientists better understand hypersomnias and their treatment. For more information:
Volunteering for clinical trials may allow you to try medicines that aren’t yet available in your home country nor approved for your diagnosis. Some clinical trials allow participants to continue taking the medicine for a period of time after the trial has ended. Clinical trials also help scientists better understand hypersomnias and their treatment. For more information:
Ask your doctor about clinical trials that are testing medicines in people with hypersomnias
Visit our “Currently-Recruiting Research Studies” web page to see a list of clinical trials and other types of research studies looking for volunteers
Building a great working relationship with your doctor is key to finding the best possible treatments for you. To find out more about preparing for appointments and communicating with your doctors, visit our web page “Finding and working with doctors who treat hypersomnias.”
Some people with hypersomnias may have other health problems that make their symptoms worse. Ask your doctor to screen you for these, such as:
Other sleep disorders, such as obstructive sleep apnea, circadian rhythm disorders, or rapid eye movement (REM) sleep behavior
Ask your doctor if the Patient Health Questionnaire-2 (PHQ-2) is right for you
Other screening tests such as the PHQ-9 may show false results due to questions about fatigue, trouble concentrating, and disrupted sleep
Autonomic dysfunction, which can include symptoms such as palpitations, headache, or dizziness
If blood loss is caused by your period (menstruation), ask your doctor about continuous hormone therapy (such as birth control pills, IUD, implant, patch, or vaginal ring) which can help limit the menstrual bleeding that can cause iron deficiency anemia and fatigue
Cardiovascular health, which may be at higher risk
If you have this, hormone therapy may help your hypersomnia symptoms
To give your hypersomnia medicines the best chance of helping your symptoms, avoid other medicines and substances (such as opioids and alcohol) that can worsen daytime sleepiness
Visit our “Quality of life tips” web page for more ideas on improving your general physical and mental health, including links to support groups
Published Apr. 22, 2020 |
Revised Feb. 1, 2024
Complete update Jan. 19, 2024 |
Approved by our medical advisory board